An increasingly common form of skin cancer
Malignant Melanoma Explained
What is malignant melanoma?
Malignant melanoma is a form of skin cancer that develops in the melanocytes, the pigment-producing cells that give skin its colour. Unlike many other skin cancers, melanoma can spread to other parts of the body if not detected and treated early.
Who gets melanoma?
Excessive exposure to ultraviolet (UV) light, from sunlight or sunbeds, is the most significant cause of melanoma. Getting sunburnt, particularly in childhood or the early adult years increases the risk later in life.
A small proportion of people may have a genetic predisposition, meaning melanoma can run in families, though this link is not yet fully understood. Individuals with weakened immune systems, such as those taking long-term immunosuppressant medication after an organ transplant, are also at higher risk.
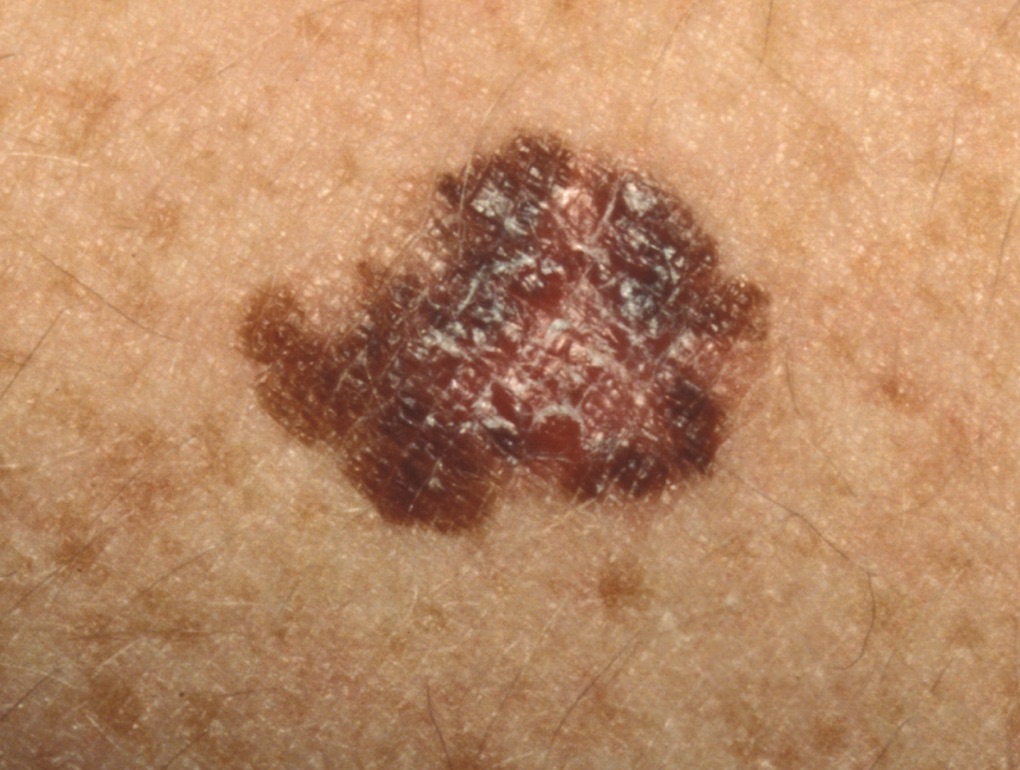
What does melanoma look like?
Melanoma can appear in many forms, and diagnosis is not always straightforward. It is best assessed by a dermatologist experienced in recognising subtle differences between harmless moles and potentially cancerous ones.
The main types of melanoma include:
Nodular melanoma:
A rapidly growing, often dark-coloured lump that may vary in colour and occasionally bleed or become tender. It may arise from a new area of skin or an existing mole.
Superficial spreading melanoma:
The most common type. Appears as a flat or slightly raised patch that is uneven in colour and has an irregular outline.
Lentigo maligna melanoma:
A slow-growing form that typically occurs on the face, often beginning as a brown patch that gradually changes in colour, shape, or size.
Acral lentiginous melanoma:
A rare type that develops on the palms, soles, or under the nails.
Melanoma can also develop in other organs of the body, although the skin is the most frequent site.
How is melanoma treated?
The main treatment for melanoma is surgical removal.
Any mole or lesion that appears suspicious should be fully excised (removed) by a consultant dermatologist experienced in skin surgery. The removed tissue is then examined under a microscope to confirm the diagnosis, identify the melanoma type, and assess how deeply the cancer cells have penetrated the skin. This is known as the Breslow thickness.
What happens after diagnosis?
All confirmed melanomas are reviewed at a specialist multidisciplinary team (MDT) meeting. This includes your dermatologist, a pathologist, surgeon, and oncologist specialising in melanoma. Together, they decide on any further treatment or follow-up care needed.
All patients require an additional operation called a Wide Local Excision (WLE). This procedure removes a rim of normal skin around the original site to reduce the risk of recurrence. It may be carried out by your consultant dermatologist or a plastic surgeon, depending on the melanoma’s location.
The management plan depends largely on the melanoma’s depth:
Thin melanomas (less than 0.8 mm)
Usually only require a wide local excision and regular follow-up.
Thicker melanomas (more than 0.8 mm)
In addition to the wide local excision, you may be offered a Sentinel Lymph Node Biopsy (SLNB). This checks whether melanoma cells have spread to nearby lymph nodes.
Further investigations
In some cases, CT scans or other imaging tests are advised to assess whether the disease has spread.
If melanoma has spread, treatments such as immunotherapy or targeted therapy may be offered through the NHS.
What is the outlook?
The prognosis depends on the depth of the melanoma at diagnosis. Around 95% of people with thin melanomas (less than 0.8 mm) make a full recovery with no further problems. Overall, about three-quarters of patients treated for melanoma do not experience a recurrence. Early detection and prompt treatment significantly improve outcomes.
Will I need follow-up appointments?
Yes, regular follow-up is essential to monitor healing, check for recurrence, and identify any new skin cancers early.
Thicker melanomas (greater than 0.8 mm):
Seen more frequently, typically for up to 5 years, under shared care between your consultant dermatologist, plastic surgeon, or oncologist.
Thin melanomas (less than 0.8 mm):
Usually reviewed every 6 months for the first year.
Your dermatologist will also advise on skin self-examination and sun protection, helping to reduce the risk of developing further melanomas in the future.