Skin rashes in intimate areas
Vulval Skin Conditions
What are vulval skin conditions?
Vulval skin conditions are disorders that affect the skin of the vulva, perineum and perianal area in women and girls of all ages. They can cause itching, soreness, burning, or pain, and may make everyday activities such as sitting, cycling, passing urine, or sexual intercourse uncomfortable. Although these problems can be distressing, most have identifiable causes and respond well to appropriate dermatological treatment once diagnosed correctly.
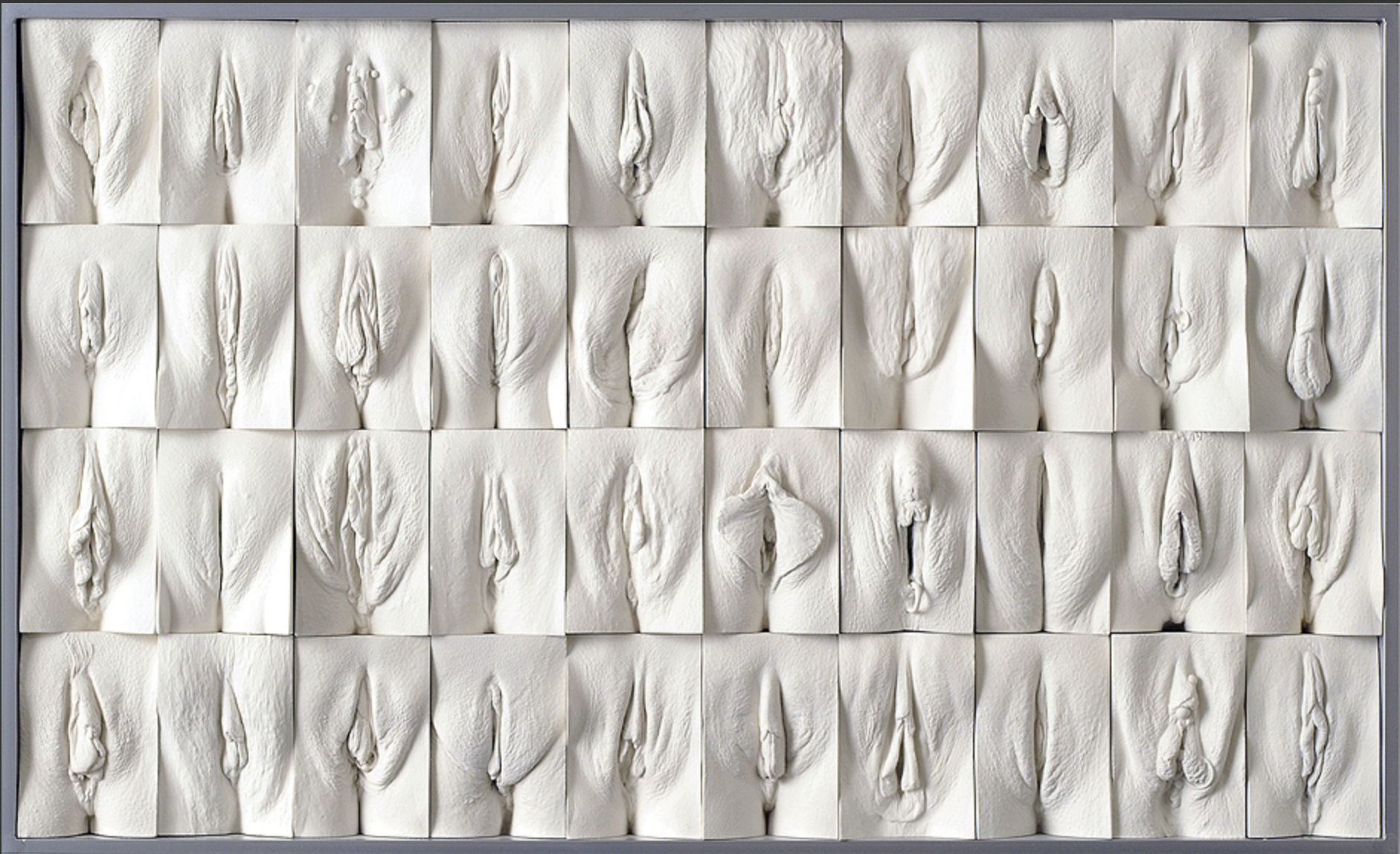
What types of conditions can affect the vulval skin?
Many different conditions can affect this delicate area. The most common seen by dermatologists include:
Eczema (dermatitis)
This can be atopic eczema (linked with allergies such as asthma or hay fever), allergic contact dermatitis (triggered by an allergic reaction to a substance touching the skin), or irritant contact dermatitis (caused by soaps, wipes, urine, or friction).
Seborrhoeic dermatitis
A common, mild condition that can cause redness, scaling and itching in skin folds.
Psoriasis
May affect the vulva as part of general psoriasis, though lesions are often smoother and less scaly in this area.
Lichen planus
An inflammatory condition that can cause soreness, redness and white streaks, sometimes associated with lichen planus elsewhere on the body.
Lichen sclerosus
A chronic condition that causes white, thin, and fragile skin, often with itching and soreness. It can also affect the perianal skin.
Vulval pigmentation
This may include benign causes such as labial melanosis or post-inflammatory pigmentation, but occasionally pigmentation changes can be a sign of systemic disease or, rarely, vulval melanoma.
Because the vulval skin is sensitive and reactive, conditions often overlap or mimic each other.
Accurate diagnosis and careful management are essential to ensure proper treatment and to avoid unnecessary discomfort.
What should I do if I think I have a vulval skin condition?
If you are experiencing symptoms such as itching, soreness, pain, or visible changes in the vulval skin, you should speak to your GP or dermatologist.
Diagnosis can be challenging and requires a detailed history, including:
Previous treatments and how your skin has responded
Any previous gynaecological procedures
Full examination of the vulval and surrounding skin as well as a full skin examination
In most cases, vulval skin conditions can be diagnosed clinically by a dermatologist without the need for invasive tests. However, a skin biopsy may occasionally be needed if the diagnosis is uncertain, if there has been a poor response to treatment, or if there is concern about a precancerous or cancerous change.
If allergic contact dermatitis is suspected, patch testing may be arranged to identify possible allergens.
Summary
Vulval skin problems are common and often treatable once properly diagnosed. Because symptoms can overlap, specialist assessment is important to ensure appropriate investigations and treatment.